By David Tuller, DrPH
Every year, Jennie Spotila deconstructs NIH funding on her Occupy M.E. blog. Last November 7, she crunched the numbers for the 2019 fiscal year, and the same day posted another blog with a more urgent message. I am re-posting that blog in full (a bit late), with Jennie’s permission.
**********
NIH Funding for ME Needs Life Support
Fiscal year 2019 is over, and we can now examine how much NIH spent on ME research.
In previous years, I’ve broken down the funding at a granular level. I have done that in a separate post for those who want the details. But as I analyzed the numbers this year, I realized that funding for investigator-initiated research needs immediate life support, or the future of ME research is grim.
Bottom line: Funding for individual grants has dropped 25% since 2017. To understand why this is a problem, we need to start by understanding the different ways NIH spends and counts research dollars.
For our purposes, NIH research spending on ME research falls into three categories. First, there is investigator-initiated research, which means a researcher receives funding for a specific project. Second, there are the Collaborative Research Centers created in 2017. These Centers are conducting multiple projects and building research infrastructure. Third, there is intramural research done at NIH itself, such as the Clinical Care Study.
NIH adds these three categories of spending together and reports funding as a single number. That annual funding number is what NIH focuses on publicly, such as in the Categorical Spending Chart or in the NANDS Working Group Report. NIH points to increases in the number as evidence that it is improving ME research. When the number goes down, NIH frequently blames it on a low number of grant applications.
In 2018, NIH spent just under $12.8 million on the three categories of research spending (see note 1). In 2019, NIH spent $12 million on two categories: investigator-initiated research and the Collaborative Research Centers (see note 2).
The change from 2018 to 2019 is relatively small: a decrease of about 6%. That sounds pretty good, right? If we look at the total amount NIH has actually spent in the last five years on ME, we see this:
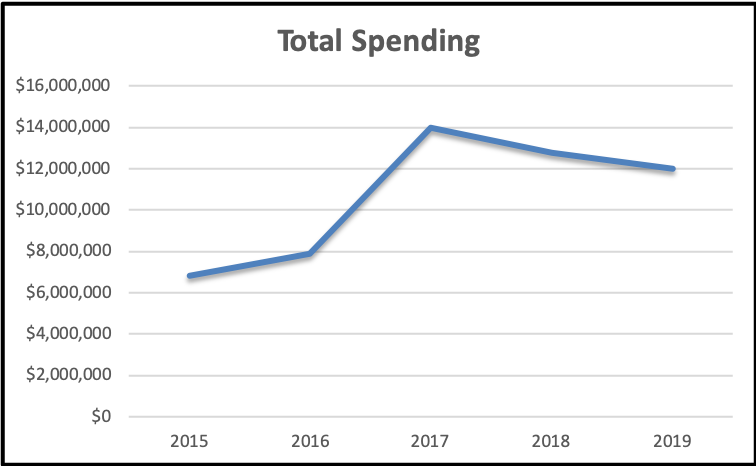
Obviously, 2017 was the high watermark of funding because it was the first year of the Collaborative Research Centers. Yet even with the decreases since then, spending is still substantially more than before the Centers were created. That should be good news.
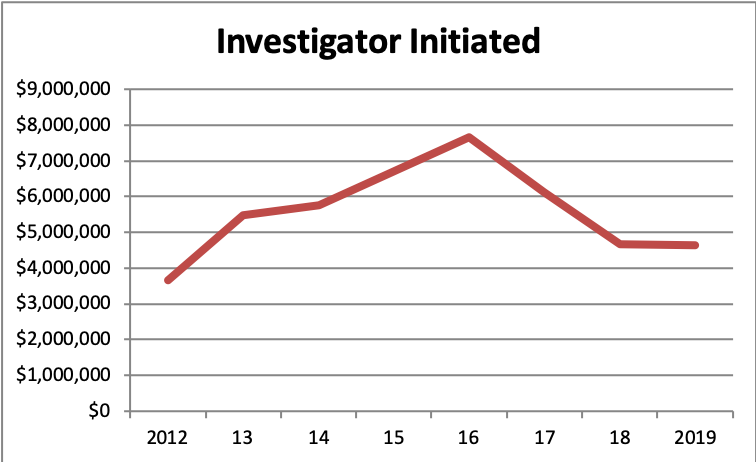
However, focusing only on the total spending ignores where the money is going. When I examined the different types of spending, I found that the investigator-initiated category has dropped sharply since the Collaborative Research Centers were created. In 2017, NIH invested $6.1 million in investigator-initiated grants. In 2019, NIH invested $4.6 million (same as in 2018).
That is a drop of 25%. In fact, investigator-initiated funding is at its lowest since 2012.
You might be wondering: If NIH funding overall is increasing, what difference does it make if the money is going to the Collaborative Research Centers instead of investigator-initiated grants? The answer is that it makes a huge difference, not only right now but it could have dire long-term consequences for ME research.
A healthy research ecosystem needs diversity in ideas, personnel, and scientific approaches. We cannot predict where the best ideas or breakthroughs will come from. For example, in ME research, not everyone should be investigating the immune system. We need projects on neurology, dysautonomia, metabolism, and so much more. We need early stage investigators, and mid-career, and established experts. We need the longstanding giants and people who are new to the field. We need collaborative teams and we need individual labs. When all of these elements are in balance, and there are adequate resources, the research field can thrive.
Since 2017, NIH funding has emphasized the Collaborative Research Centers over the individual investigator grants. NIH points to the benefits to the Research Center model, with multiple projects organized around a central theme and research group. Dr. Koroshetz explained in 2017 that the Centers are not the solution but seeds that will eventually grow the research.
There are two big problems with this approach. First, and most obvious, is that this approach takes time that we do not have. The second problem is the negative consequences of concentrating resources at three institutions rather than supporting a wider portfolio of research.
We already face a severe scarcity of resources in the ME research ecosystem. For thirty years, we have not had enough money, and so we do not have enough scientists or institutions involved in research. When NIH funded the Collaborative Research Centers, it added new money to the field but it is concentrated primarily at Columbia, Cornell and Jackson Labs. These three institutions alone received more than 57% of the entire 2019 spending. In the short term, that means those three Centers are doing the most NIH funded research, training new investigators, and publishing data.
However, as investigator-initiated funding falls, then the ME field increasingly narrows down to those three Centers and collaborators. That means an individual investigator who is not at one of those three places could have a harder time getting funding. We will lose the diversity of ideas and scientists and trainees that come from funding many different labs. Unfunded investigators will leave the field. Our pool of experts for grant review will shrink further. The Centers can do a great job training early career scientists, but if those investigators can’t get funding to start their own labs, they will probably leave the field too.
Concentrating resources disproportionately at the Centers is also dangerous because it leaves the field vulnerable to crashing. NIH funded CFS research centers in the 1990s. By 2003, that funding was terminated, the Centers disbanded, and overall funding dropped 23% in a single year. Today, the Centers represent such a huge proportion of the research portfolio that if NIH decided to terminate them tomorrow, our funding would drop by more than 60%.
We need the entire ME field to grow, but not at the expense of one type of funding over another. ME research needs the Collaborative Research Centers AND investigator-initiated funding. The significant drop in individual grant funding since 2017 is a sign that we need life support, not patience while NIH waits for the Centers to stimulate the field.
NIH is a large institution, and large institutions don’t change course on a dime. But sometimes it seems like very few people at NIH even recognize the need for significant change. A case in point is the NANDS Working Group report. The Working Group spent a year creating the recommendations in that report, and not a single one addressed the urgent need for more funding. (Read my hot take on that report)
Cort Johnson reported that after the Advisory Council of NINDS voted to accept the Working Group report, several members of the Council told Dr. Vicky Whittemore that, “they had no idea ME/CFS was so underfunded, that so little research had been done, and that such big needs were present.”
How? Is? That? Possible?
The NINDS Advisory Council voted to approve the concept of the Research Center RFA. The Council voted to create the NANDS Working Group. This was not the first time Council heard about ME/CFS or the dire funding situation, not by a long shot. I bet if I went back through the meeting videos, I could find multiple times when it had been discussed in presentations. Furthermore, the Council has previously voted to approve funding for ME grants (every Institute Council votes on grants). So how is it possible that Council did not know?
NIH consistently says that they do not receive enough grant applications, and that the ME community must do more to stimulate research. However, the burden of increasing research funding should not be placed on the people with the disease. NIH’s neglect and, in some cases, active disbelief of ME has led to the situation we are in today. NIH must take all necessary steps to correct it.
This is an extraordinary situation, and one that is very much of NIH’s own making. NIH’s persistent failure to invest the resources necessary to grow this field is how we got here. NIH needs to fix this. It is patently obvious that the field needs more Requests for Applications with set aside funding. We know that RFAs attract an increase in applications. We cannot afford to wait for the Centers to stimulate more applications five, ten, or twenty years from now. We need more funding now. We need more Research Centers now. We need more investigator-initiated grants now.
NIH is not doing enough. The NANDS Working Group report is not enough. NIH’s current investment in ME research is not enough. Dr. Koroshetz and Dr. Collins could be heroes. They have a chance right now to stop the research free fall and get us back on the right track. They have to do this, or people with ME will suffer even more.
Note 1: Note that NIH calculates the aggregate number differently than I do, because I do my best to exclude amounts that were not actually spent on ME research, as in my 2018 Fact Check post.
Note 2: NIH won’t release its numbers for intramural funding until next spring (and those numbers are not always accurate), so for now we have to rely on just the numbers that are publicly available.
Comments
6 responses to “NIH Funding “Needs Life Support,” Says Jennie Spotila”
Why should the NIH waste money funding “ME/CFS” research?
Cort Johnson of Simmaron Research says patients just need to do
the Annie Hopper brain-retraining program.
https://www.healthrising.org/blog/2020/01/05/christines-dnrs-chronic-fatigue-recovery-story/
David, did you know that NIH doesn’t list a prevalence figure for ME/CFS on it’s spending by disease page, but does for other diseases with high numbers of patients? Would be a good topic for you to follow up on to increase awareness within NIH.
https://report.nih.gov/categorical_spending.aspx
For those wanting to look it up the disease is listed in the table as “Chronic Fatigue Syndrome (ME/CFS)”, and prevalence is the last column
This administration is not interested in SCIENCE. Therefore, no push from the top.
They love to cut funding – we and our research needs are an easy target.
We are like AIDS patients – having to push the medical community because most of them have no interest in us. AIDS patients, after MANY deaths, prevailed (probably because the world found out that people other than gay men could get AIDS). I’m still ashamed of the way they were treated by doctors, the government, and by society at large.
I don’t understand why. I’m living my life as best I can treating symptoms as best I can, and not having the energy to be an activist (bless all of those who do), with my only contribution being some funds and a novel with an ME/CFS main character, which I can’t get many people to read – but when they do, give me all kinds of compliments.
Medical research is NOT my bag. I don’t have anything to help with – I used to be a research physicist.
My government has failed me and is continuing to do so, lickety split. The people who manage the government funding continue to lie and pretend they are doing something.
PS I could not comment on Jennie’s blog; I have resubscribed because I used to get these posts – and seem to have gotten lost somehow from their list. One step forward, three steps back.
Which makes this recent article from the AP on the NIH study all the more infuriating. https://apnews.com/4bc281b36227afb674649cdf9f137be2
They claim a budget of over $14 million for ME/CFS. Koroshetz says, “The ignorance about the condition just vastly dwarfs what we know about it.”
Whose fault is that?