By David Tuller, DrPH
*October is crowdfunding month at Berkeley. I conduct this project as a senior fellow in public health and journalism and the university’s Center for Global Public Health. If you would like to support the project, here’s the place: https://crowdfund.berkeley.edu/project/22602
The pandemic has played havoc with everything, including the timeline of the development process for the new ME/CFS guidance from the UK National Institute of Health and Care Excellence. Originally, a draft of the guidance was supposed to be released earlier this year. Following a period of public comment, NICE planned to issue the final version by December. Under the new schedule, the draft version is being released in November, with a six-week comment period to follow. The final version will be released next April.
To recap: The current guidance, which was issued in 2007, recommends cognitive behavior therapy and graded exercise therapy for what was then being called CFS/ME. The committee was dominated by members the CBT/GET ideological brigades. Three years ago, NICE preliminarily decided not to revise the guidance–and then reversed itself after enormous pushback. The process of appointing the new committee took place under enormous public scrutiny. The committee ended up including both people who believe in proper science and CBT/GET ideologues, so predicting the outcome is a challenge.
In the minutes of its September board meeting, the group Forward-ME included an update from Charles Shepherd about the status of the NICE guidance development. Shepherd is the ME Association’s longtime medical director and has been involved with the process. Here’s what the minutes noted:
Charles stressed that this was going to be a completely new guideline. There had been many Zoom meetings during July and August and had made up the ground lost during lockdown. A draft with conclusions and recommendations had been produced and consensually agreed. The draft would go out to Stakeholder consultation on 10 November and there would be a 6-week consultation period ending on 22 December.
I’m not sure if that means the role of the guidance committee and its members is essentially already over. But from what I understand, NICE committee members are supposed to hold their tongues and not tweet out public pronouncements about matters that have been under deliberation. That’s why it was surprising that one member of the ME/CFS committee, Bath psychologist Jo Daniels, tweeted the following on Wednesday:
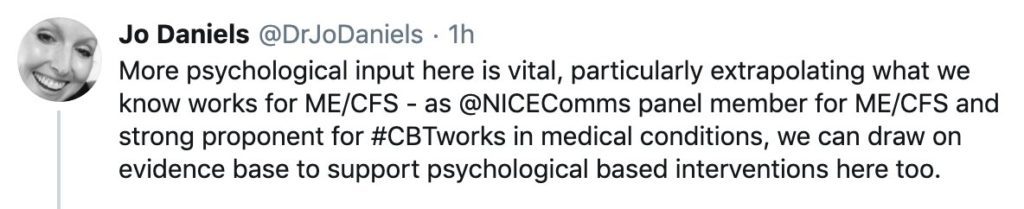
As a reminder: Earlier this year, Daniels and colleagues published a study that purported to prove the effectiveness of a specialized form of CBT for CFS/ME patients with “co-morbid severe health anxiety.” (I critiqued the study here.) Even though it is normal for patients to experience anxiety about a complex medical condition that clinicians tend to dismiss, the investigators posited it as an independent psychological problem that should be targeted for intervention. This study appeared designed to generate a funding stream for more research into “CBT-for-health-anxiety” as an treatment for anxious CFS/ME patients, but the argument disintegrated under scrutiny.
Now Daniels appears to have engaged in public advocacy on an issue before the NICE guidance committee. According to the tweet, “we know” CBT works as a treatment for ME/CFS—that is, despite international repudiation of the PACE trial and its associated treatment paradigm. The tweet has since been deleted. Maybe Daniels realized she might have crossed a line, given her position as a NICE committee member. Oops!
No worries. The tweet was captured in screen shots.
The new guidance–if it’s any good–couldn’t come soon enough, given some confusion over the applicability of the 2007 recommendations to prolonged symptoms after acute Covid-19. During the summer, NICE issued a statement warning against the assumption that the 2007 recommendation for GET also applies to patients with post-Covid symptoms. (The NICE statement did not similarly warn against CBT for post-Covid symptoms. It’s hard to read the tea-leaves, but perhaps that means GET is on shakier ground in the forthcoming draft than CBT. Or maybe not.)
Yet in a recent webinar hosted by the Royal Society of Medicine about these “long-Covid” symptoms Liverpool physician Alastair Miller cited the NICE guidance for CFS/ME in advocating GET. He did not mention the NICE advisory about this very matter. He also did not mention that NICE is developing new guidance because of widespread recognition that the one he cited in the webinar is deficient. Hey, Alastair–keep up!
Comments
10 responses to “NICE Draft Guidance on ME/CFS Coming Next Month”
It gets to me that people are calling it ‘LONG-Covid’ now rather than just ‘post-covid syndrome’ when, compared to ME, sufferers have had the continuing/lasting symptoms for such a comparably short time. Perhaps ME sufferers should start calling their condition ‘Long-ME’, or ‘Very Long – ME’, or “Interminably Long-ME” in the case of those who have endured it for decades? Maybe that would help to get into NICE’s thick skulls how much ME patients are suffering and have suffered as a consequence of their previous guidelines.
Yesterday I saw an item on the national news about ‘Long-Covid’. The presenter concluded the item by saying that it was ‘paramount’ that the condition was taken seriously, or words to that effect. (Of course it is, I wouldn’t disagree with that.) But it’s paramount too that NICE revises its guidelines on ME/CFS and stops recommending that patients are shunted off into CBT and GET instead of getting the investigations and biomedical care that they so desperately need.
CT: couldn’t agree more! For myself I’m not sure the ““Interminably Long-ME”” moniker quite suffices either. For those with post-covid pondering their futures, it might not be that encouraging to know that some of us have been ill for (literally) half a century. And during that time ‘I’ have met with very little care but a great deal of gaslighting which has continued to this very week. Maybe if those with post-covid ponder this possibility they might not only shout out for their own care based on a belief and understanding of their symptoms, but also rally a cry on behalf of people with ME who have lived a hell of disbelief and sometimes unbearable symptoms for so very long. ‘Long’ can be interpreted in so many ways can’t it? Being ill for weeks might seem insufferable to most people, being ill for 50 years … think about that. And I’m not alone.
The equivalent would be ‘(Life)long entvid’ after the virus that causes ME. But surely post-covid disease will eventually receive a proper name. Or two, since it appears come as two distinct diseases (note: enteroviruses cause a good dozen).
As for NICE, I’m not so certain that the new guidance will be an improvement, since its starting point is an imaginary illness. Is anyone better off if CBT/GET is replaced with spinal surgery, for instance?
The tweet referenced above was one of two deleted tweets by Daniels. The second was:
2020-10-06 12:38:17
“@EddCarlton @trishgreenhalgh @NICEComms Furthermore, long-haul COVID is likely to be distressing & reduce quality of life as well as physical functioning, all of which are amenable to evidence based psych therapies; more than half with LTC experience mental health problems – we must put support in place for this here.”
X !! Oh my..this stuff would be laughable if it wasn’t so serious. Land grab of epic proportions based on thin air. Suddenly all these recently, otherwise healthy, people with ‘Long Covid’ are now experiencing mental health problems are they? What evidence exists that they are? Ridiculous. The shame is that people with definable mental illnesses are shouting out for care that is not forthcoming. RCPsych need to stop meddling in stuff we know to be way outside their ken and get down to looking after those patients who really need their help.
Ask the Long-Covid patients if they want psych therapy. Some may want it, some may not, but I’ll wager that 99.99% of them will want good biomedical care and the bulk of the funding to go into that.
Worth pointing out again that much of the ‘depression/anxiety’ seen in ME/CFS, postSARS, longcovid is in fact not depression, but misuse of depression and anxiety instruments. HADS, for example will misread physical inability for depression/anxiety. It assumes you are healthy.
There are papers out there for longcovid/PTSD that do the same.
For example, https://pastebin.com/zeC9Fsqe – assumes physical return to pre-morbid state. If this is not true, many (3,8,10*,11,15,17,18,19) of the 19 questions may assume PTSD when it’s physical or reaction to physical ongoing symptoms.
If I’m ‘not enjoying things I used to’ – that can mean I can’t do them as well as I don’t enjoy them.
Ian Stirling: very good point and a hazard in all BPS / ‘CFS/ME’ ‘research’ that uses HADS too (probably most of it).
While my daughter lies in bed 24/7, life devastated by ME (20yrs & counting) we live in fear of medical professionals and find it hard to have faith in NICE improving anything. Thank you David for your continued support. I won’t waste my time with my opinion on the psyche brigade continuing to ……. peoples lives. The only positive i see is the biomedical research being moved on by ME Researchers looking into similarities with long covid. The psyche brigade have their eyes on the money, please please don’t let this happen.
My broken brain remembers (incorrectly?) that “depression” and “anxiety” are two different symptoms that feel very different. But now it’s always “depression-and-anxiety” or “anxiety-and-depression”.
How and when did this happen? Is it because the same mostly useless drugs and mostly useless CBT are prescribed for either symptom?